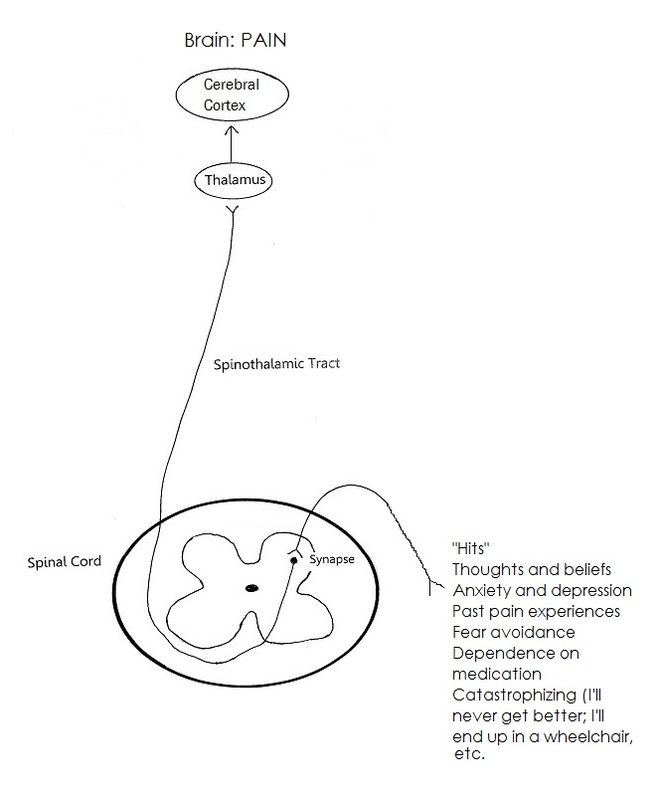
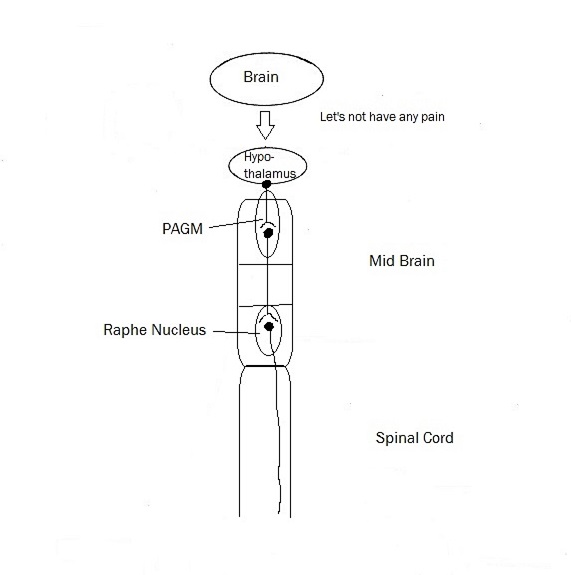
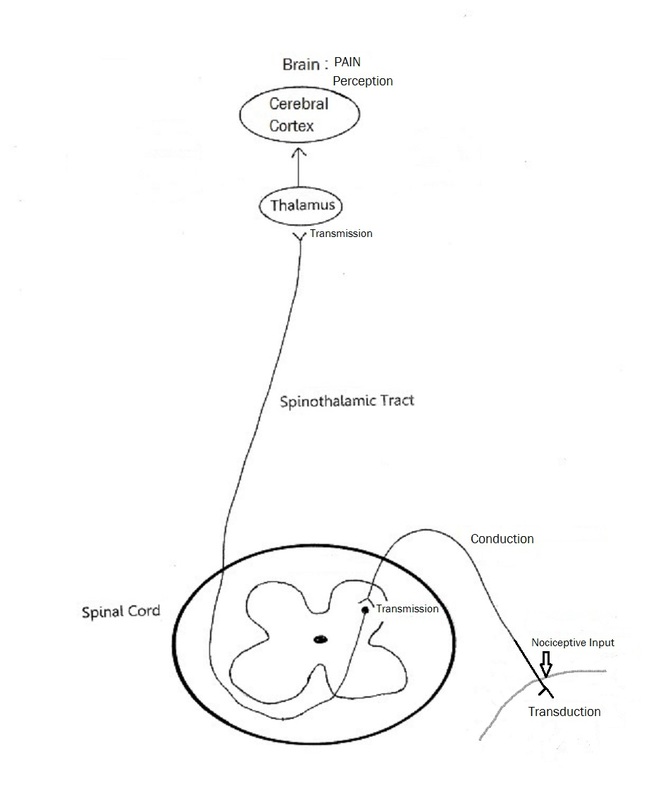
- Any credible evidence of danger to your body will modulate pain.
- Related tags share neurons (neurotags). Take back pain for example:
- Beliefs about your back
- Thoughts and feelings about your back
- Neurons that fire together, wire together.
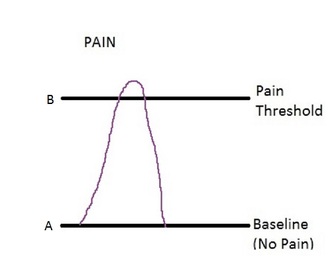
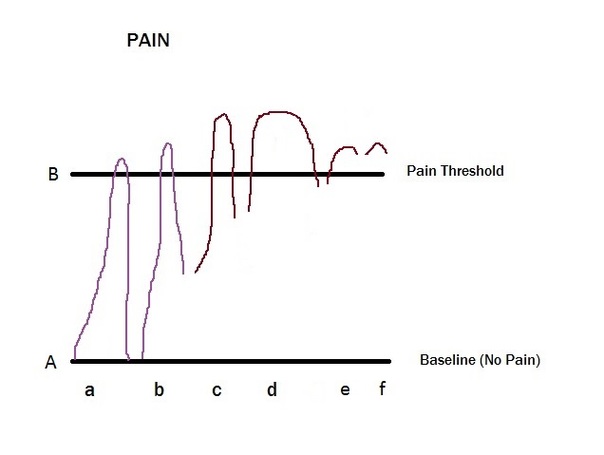
- When pain persists:
- there is increased sensitivity, i.e., the neurotag that produces your back pain is more sensitive, such that even just watching someone pick up a box would make your back hurt (this pain has been picked up in brain scans, so we know that subjects are not lying about their pain) --the network or pain pathway, if you like, becomes stronger and stronger. (The more you feel pain, the better your body becomes at producing it--it is reinforcing the neural pathway to producing pain). It is the familiar road with the well-trodden path, it is "all roads lead to Rome" (pain). Sometimes thoughts, sometimes smells, foods, images, sounds, etc can lead to pain. They share the same neurotag that results in pain.
- there is decreased precision: the area over which you feel pain becomes diffuse, and hard to pinpoint.

 RSS Feed
RSS Feed